
CAR-T cell therapy is transforming the way leukemia is treated, especially in cases where the disease returns or resists standard treatments. By reprogramming T cells to recognize and attack leukemia cells, this advanced immunotherapy has helped some patients achieve lasting remission.
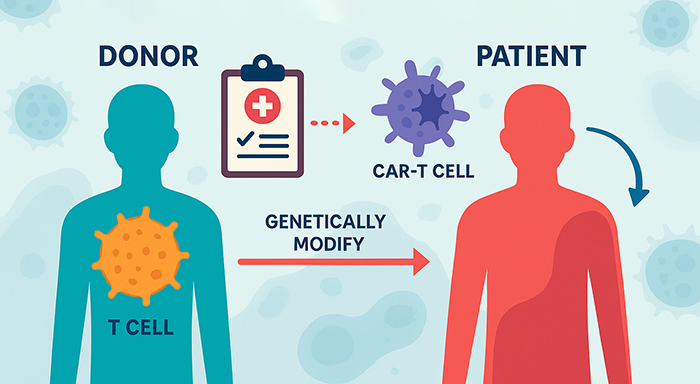
While autologous CAR-T therapy—which uses the patient’s own T cells—is more common, there are situations where donor-derived CAR-T therapy (also called allogeneic CAR-T) becomes the better or only option. This article explains when and why this alternative approach is considered.
What Is Donor-Derived CAR-T Cell Therapy?
Unlike traditional CAR-T therapy, which uses the patient's own immune cells, donor-derived CAR-T relies on T cells from a healthy donor. These cells are engineered to target cancer-specific markers and then infused into the patient. This option is especially helpful for individuals whose immune system has been heavily weakened or altered.
When Should Donor-Derived CAR-T Be Considered?
- Leukemia Recurrence After Allogeneic Stem Cell Transplant (HSCT)
Patients who relapse following a stem cell transplant may benefit most from donor-derived CAR-T therapy. Because their immune system is already based on donor cells, this type of CAR-T is less likely to be rejected. Clinical studies have shown impressive results: for example, a Phase I trial reported a 70% complete remission rate in patients with B-cell acute lymphoblastic leukemia (B-ALL) who relapsed after HSCT. - Inability to Use Autologous T Cells
Some patients, especially those who’ve had extensive prior treatments, have T cells that are too damaged or depleted for harvesting. In these cases, using T cells from a donor provides a healthy, functional alternative that can be genetically modified and expanded more effectively. - T-Cell Leukemias (e.g., T-ALL)
Donor-derived CAR-T therapy has also shown promise in rare blood cancers like T-cell acute lymphoblastic leukemia (T-ALL). When designed to target the CD7 antigen, these therapies have produced sustained responses in a portion of patients. A 2-year follow-up showed that 60% of treated patients remained in remission, although relapse remains a risk.
Benefits of Donor-Derived CAR-T Therapy
- Lower Risk of Rejection: The immune compatibility with prior transplant recipients allows donor CAR-T cells to integrate and function better.
- Longer Persistence: These modified immune cells can stay active in the body for months or even years, helping prevent future relapse.
- Faster Treatment Availability: Donor T cells can be pre-collected and stored, speeding up treatment when immediate action is needed during relapse.
Safety and Side Effects
As with any CAR-T therapy, donor-derived approaches come with potential risks:
- Acute Reactions: Side effects may include cytokine release syndrome (CRS) and mild graft-versus-host disease (GVHD).
- Late Complications: Patients may experience severe infections or, in rare cases, a worsening of GVHD symptoms.
These risks are monitored closely by medical teams and are typically managed with supportive care and medications.
Future Directions in CAR-T for Leukemia
Although not used as a first-line treatment, donor-derived CAR-T therapy is increasingly vital for patients who are not eligible for autologous options. Researchers are now developing universal CAR-T therapies that could benefit a wider group of patients and extend to other conditions like acute myeloid leukemia (AML).
In summary, donor-derived CAR-T therapy is a powerful option in challenging leukemia cases. With its expanding role in relapsed and refractory leukemia treatment, this approach brings new hope for patients who have limited alternatives.
Publication date: May 7, 2025.
Sources
lls.org
pubmed.ncbi.nlm.nih.gov
thelancet.com
cancer.gov
cancer.gov
dana-farber.org
nature.com
ascopubs.org







